Random Assignment Procedure
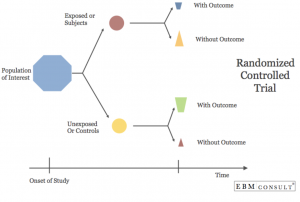
Since randomly assigning a control group that receives no treatment is unethical, the control group will be assigned based on capacity, or, the amount of open beds in the I CAN facility. In this kind of Randomized Control Trial (RCT), the pool of subjects is the amount of people entering the I CAN facility on a given day There are not always enough beds to accommodate the number of people seeking treatment, so I CAN is sometimes forced to turn people away. In this situation, when there is not an available bed for the patient, I CAN will contact other treatment facilities to find out if those facilities have room for the individual. If there is room, I CAN then provides transportation for the individual to get to that treatment center. If all other facilities also have no capacity, patients are referred to their local emergency room department. The patients that are turned away from I CAN and placed into other facilities will act as our control group. Patients who enter I CAN treatment will act as our experimental group. While perhaps more difficult to achieve, a RCT is optimal from a methodological perspective because it allows patients to be assigned to control or experimental groups with as little bias as possible. This, in turn, allows comparisons between treatment groups to be made more effectively.
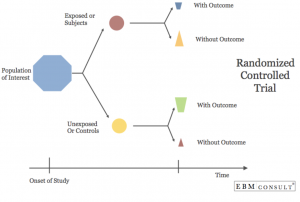 In addition, randomization eliminates the ability for individuals to manipulate the control groups. This is due to the fact that an individual is not deciding the control and treatment groups. Rather, the groups are created solely based on capacity of I CAN Recover. Lastly, monetary incentives will be offered to patients in order to encourage participation in the study. The incentives will likely be in the form of a gift card of each patient’s choice.
In addition, randomization eliminates the ability for individuals to manipulate the control groups. This is due to the fact that an individual is not deciding the control and treatment groups. Rather, the groups are created solely based on capacity of I CAN Recover. Lastly, monetary incentives will be offered to patients in order to encourage participation in the study. The incentives will likely be in the form of a gift card of each patient’s choice.
There are several addiction treatment services offered in the Hartford area. Three of the facilities patients may be sent to if there is no space at I CAN are CleanSlate, Connecticut Addiction Medicine, LLC, and Root Center for Advanced Recovery. CleanSlate and Root Center for Advanced Recovery both offer MAT and outpatient services. Connecticut Addiction Medicine, LLC is more comparable to I CAN Recover. This model offers a wide range of treatment options including MAT, psychotherapy and counseling, inpatient detox, outpatient detox, intensive outpatient programming, partial hospitalization, and three residential programs – 28 day, 45 day, and 90 day options. This model differs from I CAN because they do not focus on the whole individual, and patients are encouraged to participate in twelve step recovery.
Data Collection

Firstly, to demonstrate InterCommunity’s commitment to long-term addiction treatment evaluation, we propose a 5-year outcome measurement. Based on addiction treatment program evaluations discussed in prior literature, programs that evaluate outcomes for longer than one year report more favorable results in terms of abstinence and quality of life. I CAN Recover could benefit greatly from such a treatment model.
Patients will complete a survey upon their admittance into the treatment facility. The employee at the treatment center that is checking individuals in will first explain the study then ask the individual to sign a form of consent. The survey is the first step of the study which will collect demographic information, substance abuse history, treatment history, family history, as well as determine the best way to contact patients once they leave the facility. We recommend this survey be developed using the Addiction Severity Index (ASI). Once the patient completes their treatment, they will then be followed for five years. The patient will self-report drug use. When possible, they will do in person interviews once every three months and potentially give a urine sample. In addition, patients should report if they have gone back to treatment and if so, what facility and program. These follow-up interviews will help address not only retention rates but also ask questions that will help improve the model as best it can be based on the feedback of participants.
Outcome Measures
Effectiveness will be measured by:
- Retention rates for each treatment model
- The number of sober days per month
The retention rate of the program (not the retention rate of the study) will show how well the program is able to connect with individuals and keep them engaged and motivated with recovery. To achieve an adequate retention rate, we propose that InterCommunity establish a goal of 70 percent retention. This means that at least 70 percent of study participants remain in treatment throughout its duration. Setting such an ambitious goal will incentivize the InterCommunity staff to find ways to keep participants engaged during treatment over a long-term basis.
In addition, measuring the number of sober days will measure if an individual has increased, decreased, or not changed the amount that they use drugs. This is beneficial because it will show if facilities are reaching their goal of having patients decrease use after leaving treatment. I CAN’s outcomes will then be compared to the outcomes of the other treatment models in the Hartford area in addition to the data derived from InterCommunity health before I CAN was implemented.